Comprehensive Review of Acute Primary Angle Closure: Etiology, Diagnosis, Treatment, and Recent Innovations
Abstract: Acute primary angle closure (APAC) poses a significant ophthalmological emergency, necessitating prompt diagnosis and intervention to prevent irreversible vision loss. This article offers a comprehensive review of APAC, exploring its etiology, clinical manifestations, diagnostic modalities, treatment strategies, and recent advancements in the field. By enhancing our understanding of APAC, ophthalmologists can improve patient outcomes and mitigate the devastating consequences of this sight-threatening condition.
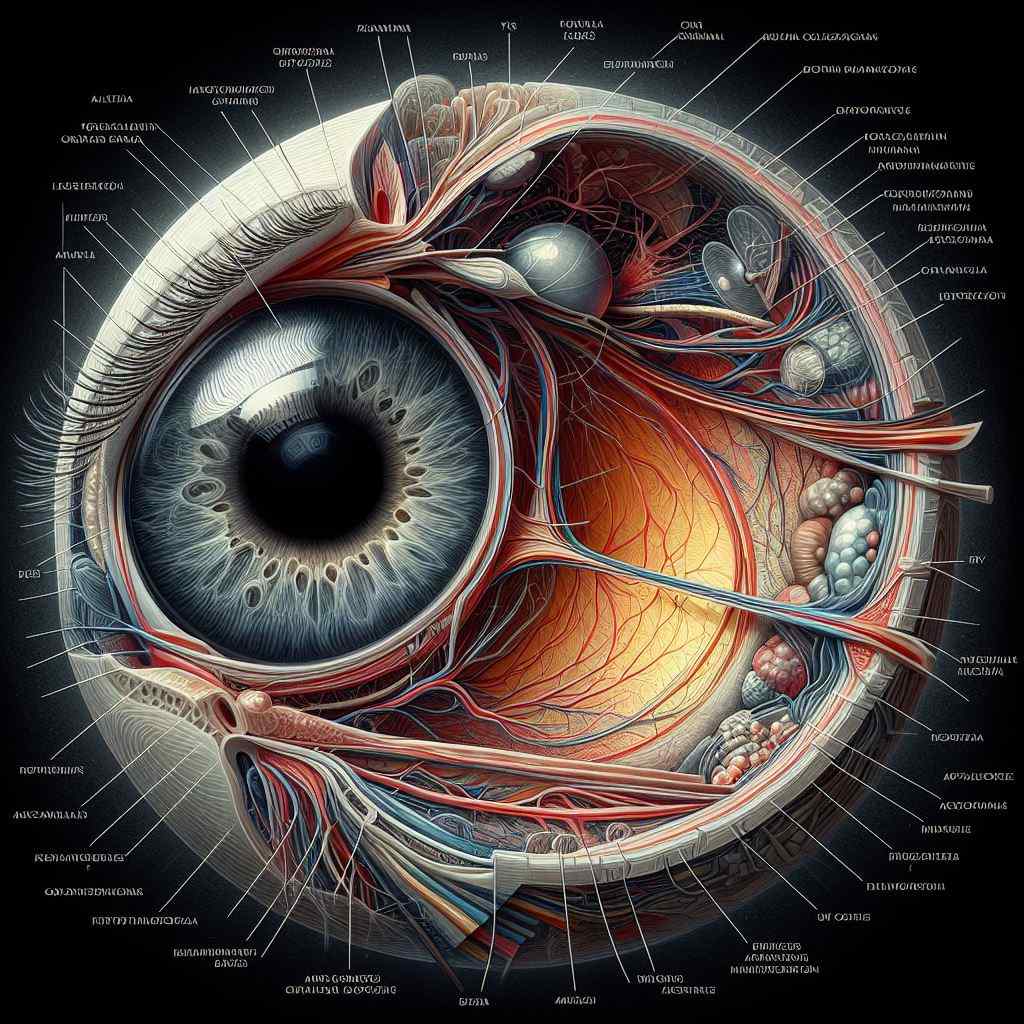
Introduction: Acute primary angle closure represents a critical ophthalmic condition characterized by sudden elevation of intraocular pressure (IOP) due to blockage of the iridocorneal angle. This acute rise in IOP can lead to rapid and severe damage to the optic nerve, resulting in irreversible vision loss if left untreated. Timely recognition and appropriate management are essential to alleviate symptoms, preserve visual function, and prevent long-term complications.
Etiology: The primary underlying mechanism of APAC involves the closure of the drainage angle, typically due to pupillary blockage or anatomical predisposition in eyes with a shallow anterior chamber. Contributing factors may include age, hyperopia, lens thickness, and anatomical variations in iris configuration. Additionally, certain medications, such as anticholinergic drugs, can precipitate an acute angle-closure crisis in predisposed individuals.
Clinical Manifestations: Patients with APAC often present with sudden onset of severe eye pain, blurred vision, halos around lights, headache, nausea, and vomiting. Physical examination may reveal a fixed mid-dilated pupil, corneal edema, conjunctival injection, and elevated IOP. Prompt recognition of these clinical features is crucial for initiating appropriate management and preventing irreversible vision loss.
Diagnostic Modalities: Diagnosis of APAC relies on a combination of clinical evaluation and specialized diagnostic tests. Key diagnostic modalities include gonioscopy to assess the iridocorneal angle, measurement of IOP using applanation tonometry, evaluation of optic nerve head morphology, and anterior segment imaging techniques such as anterior segment optical coherence tomography (AS-OCT) to visualize anatomical structures.
Treatment Strategies: Management of APAC aims to rapidly lower IOP, relieve symptoms, and prevent further optic nerve damage. Immediate interventions may include topical and systemic medications to reduce IOP, such as topical beta-blockers, alpha agonists, and carbonic anhydrase inhibitors, along with oral acetazolamide for rapid IOP reduction. Additionally, laser peripheral iridotomy (LPI) is often performed to alleviate pupillary blockage and restore aqueous outflow.
Recent Innovations: Recent advancements in the management of APAC have focused on improving treatment efficacy and patient outcomes. Emerging technologies such as microinvasive glaucoma surgery (MIGS) offer minimally invasive approaches to enhance aqueous outflow and lower IOP, providing an alternative treatment option for select patients with APAC. Additionally, advancements in imaging modalities, including AS-OCT and ultrasound biomicroscopy (UBM), enable detailed visualization of anterior segment structures, facilitating accurate diagnosis and treatment planning.
Conclusion: Acute primary angle closure represents a sight-threatening emergency that requires prompt recognition and intervention to prevent irreversible vision loss. By familiarizing themselves with the etiology, clinical manifestations, diagnostic modalities, and treatment strategies for APAC, ophthalmologists can effectively manage this condition and improve patient outcomes. Continued research and innovation in the field hold promise for further enhancing our ability to diagnose and treat APAC, ultimately reducing the burden of vision impairment associated with this condition.
For further reading and reference:
- American Academy of Ophthalmology – Acute Angle Closure Glaucoma: https://www.aao.org/eye-health/diseases/acute-angle-closure-glaucoma
- Glaucoma Research Foundation – Acute Angle Closure Glaucoma: https://www.glaucoma.org/glaucoma/acute-angle-closure-glaucoma.php
- National Eye Institute – Angle Closure Glaucoma: https://www.nei.nih.gov/learn-about-eye-health/eye-conditions-and-diseases/glaucoma/angle-closure-glaucoma


