Navigating Posterior Ischaemic Optic Neuropathy: Insights into Pathogenesis, Clinical Features, Diagnosis, and Management
Abstract: Posterior Ischaemic Optic Neuropathy (PION) presents a diagnostic and therapeutic challenge due to its diverse etiologies and elusive clinical presentation. This article provides a comprehensive review of PION, encompassing its pathophysiology, clinical manifestations, diagnostic approaches, and management strategies. By elucidating the latest research findings and treatment modalities, ophthalmologists can effectively navigate the complexities of PION, optimizing patient care and visual outcomes.
Introduction: PION poses a diagnostic conundrum for ophthalmologists, necessitating a thorough understanding of its underlying pathophysiology, clinical characteristics, and diagnostic methodologies to facilitate prompt intervention and mitigate visual morbidity.
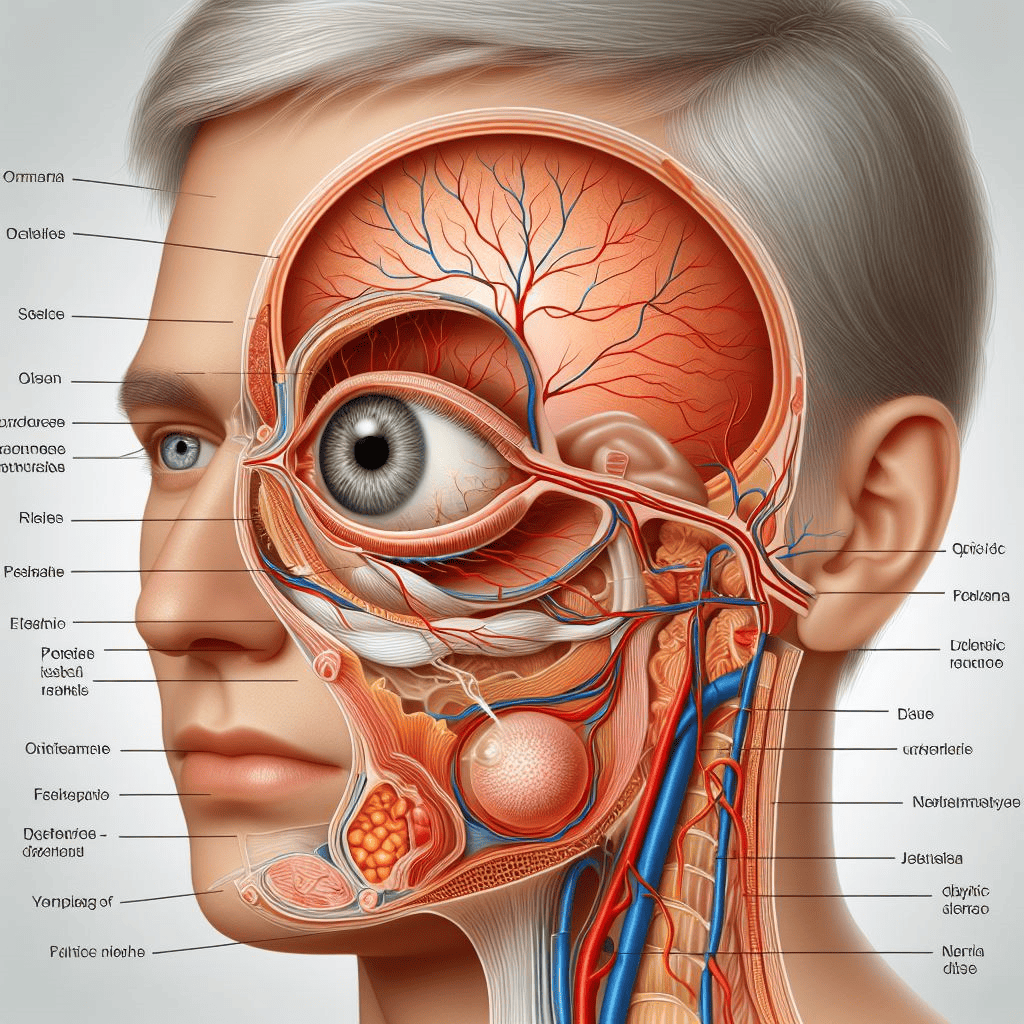
Pathophysiology: PION results from insufficient blood supply to the posterior optic nerve, leading to ischemia and subsequent optic nerve dysfunction. Etiologies include perioperative complications, arteritic processes, vascular insufficiency, and systemic diseases such as diabetes mellitus and hypertension.
Clinical Manifestations: Clinical presentation of PION varies widely and may include acute or subacute painless vision loss, with characteristic features such as relative afferent pupillary defect (RAPD), visual field defects, and optic disc pallor on fundoscopic examination. Distinguishing between anterior and posterior forms of PION is crucial for appropriate management.
Diagnosis: Diagnosing PION necessitates a comprehensive ophthalmic evaluation, including visual acuity assessment, pupillary examination, visual field testing, and fundus examination to assess optic disc appearance and associated findings. Additional diagnostic modalities such as optical coherence tomography (OCT) and neuroimaging studies may aid in confirming the diagnosis and elucidating underlying pathology.
Management: Management of PION focuses on addressing the underlying etiology while optimizing visual function and preventing disease progression. Treatment modalities may include systemic corticosteroids, vasodilators, and aggressive management of systemic comorbidities. Rehabilitation strategies such as low-vision aids and visual rehabilitation programs play a crucial role in enhancing the quality of life for affected individuals.
Conclusion: PION presents a multifaceted clinical entity requiring a comprehensive approach to diagnosis and management. By understanding its pathophysiology, recognizing clinical features, and employing advanced diagnostic and therapeutic interventions, ophthalmologists can effectively address PION, thereby improving patient outcomes and visual prognosis.
For further reading and reference:
- American Academy of Ophthalmology – Posterior Ischaemic Optic Neuropathy Overview: https://www.aao.org/eye-health/diseases/posterior-ischemic-optic-neuropathy-diagnosis-trea
- National Institutes of Health – Posterior Ischaemic Optic Neuropathy Information: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3038754/


