Exploring Other Orbital Inflammations: A Comprehensive Review
Abstract: Orbital inflammations encompass a broad spectrum of pathological entities beyond common infectious and inflammatory conditions. This comprehensive review delves into the diverse range of orbital inflammations, shedding light on their etiology, clinical manifestations, diagnostic approaches, management strategies, and recent advancements in the field. By expanding our understanding of these less common entities, ophthalmologists can enhance their diagnostic accuracy and refine treatment algorithms for optimal patient care.
Introduction: While infectious and inflammatory orbital diseases are well-documented, several less common entities pose diagnostic and therapeutic challenges to ophthalmologists. Understanding the nuances of these other orbital inflammations is paramount for accurate diagnosis and tailored management.
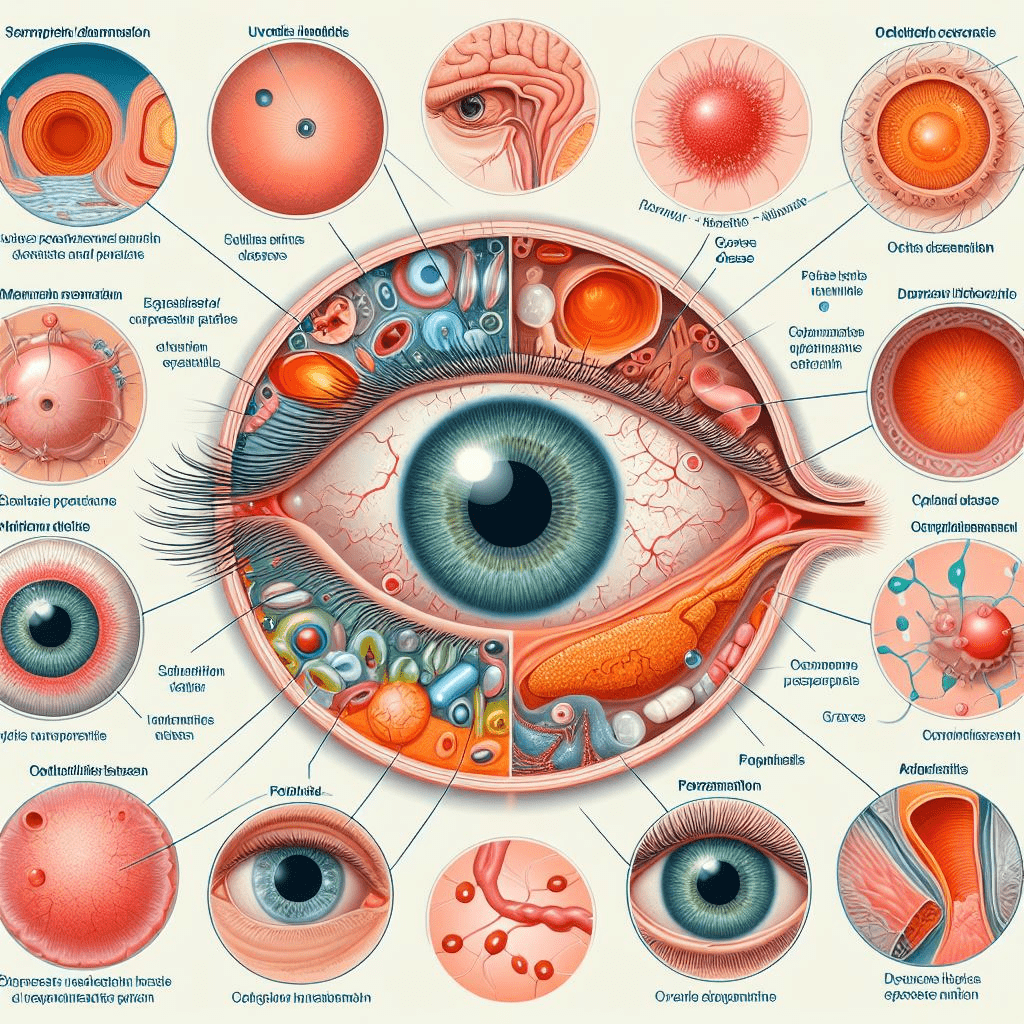
Etiology and Classification: Other orbital inflammations may arise from various etiologies, including autoimmune processes, granulomatous diseases, vasculitides, neoplastic mimickers, and idiopathic origins. Classifying these entities based on their underlying pathology aids in guiding diagnostic workup and therapeutic interventions.
Clinical Manifestations and Diagnostic Workup: Patients with other orbital inflammations may present with proptosis, pain, diplopia, visual disturbances, or systemic symptoms. Diagnostic evaluation typically involves a combination of clinical examination, imaging studies (MRI, CT), laboratory investigations (serology, biopsy), and occasionally, ancillary tests such as orbital biopsy or molecular analysis. Advanced imaging techniques like diffusion-weighted MRI and positron emission tomography (PET) have emerged as valuable tools in characterizing inflammatory lesions and assessing treatment response.
Management Strategies: Treatment of other orbital inflammations hinges on the underlying etiology, disease severity, and potential for vision-threatening complications. Therapeutic modalities encompass a spectrum ranging from observation and conservative measures (e.g., systemic corticosteroids, immunomodulatory agents) to more aggressive interventions such as surgical debulking or targeted biologic therapies. Multidisciplinary collaboration with rheumatologists, neurologists, and oncologists is often necessary for optimal patient care.
Conclusion: Other orbital inflammations represent a heterogeneous group of pathologies that pose diagnostic and therapeutic dilemmas to ophthalmologists. By staying abreast of the latest diagnostic modalities and treatment paradigms, clinicians can navigate the complexities of these conditions and optimize outcomes for affected individuals.
For further reading and reference:
- American Academy of Ophthalmology (AAO) – Orbital Inflammatory Diseases: https://www.aao.org/bcscsnippetdetail.aspx?id=f856c835-ae61-44c2-9fb9-0f9875b74604
- National Eye Institute (NEI) – Orbital Inflammation and Infection: https://www.nei.nih.gov/learn-about-eye-health/eye-conditions-and-diseases/orbital-inflammation-and-infection


