Unraveling Preseptal Cellulitis: A Comprehensive Review
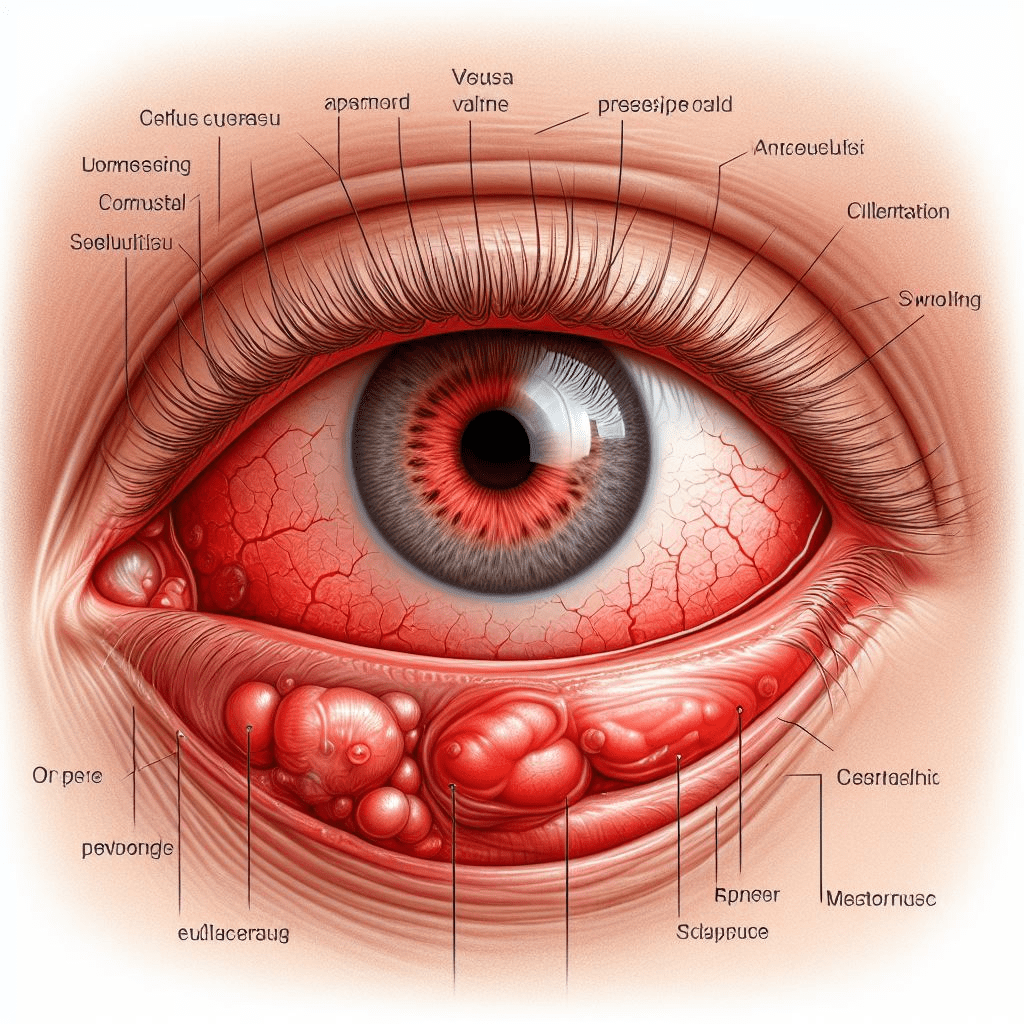
Abstract: Preseptal cellulitis, characterized by inflammation of the eyelid and surrounding tissues anterior to the orbital septum, is a common condition encountered in clinical practice. This article provides a thorough examination of preseptal cellulitis, covering its etiology, clinical presentation, diagnostic workup, management strategies, and recent advancements in the field. By elucidating the intricacies of preseptal cellulitis, ophthalmologists can effectively diagnose and manage this condition to optimize patient outcomes.
Introduction: Preseptal cellulitis, although typically less severe than orbital cellulitis, requires prompt recognition and appropriate management to prevent potential complications. Understanding the distinguishing features of preseptal cellulitis is crucial for accurate diagnosis and timely intervention.
Etiology and Pathophysiology: Preseptal cellulitis commonly arises from contiguous spread of infections originating from the face, eyelids, or periorbital structures. Common causative organisms include Staphylococcus aureus and Streptococcus species, although other bacteria and occasionally fungi may also be implicated. Trauma, insect bites, and surgical procedures can serve as predisposing factors for the development of preseptal cellulitis.
Clinical Presentation and Differential Diagnosis: Patients with preseptal cellulitis typically present with eyelid erythema, edema, warmth, and tenderness. Systemic symptoms such as fever and malaise may accompany severe cases. Differential diagnosis includes orbital cellulitis, allergic reactions, and other causes of eyelid swelling, necessitating careful clinical evaluation and, at times, imaging studies to differentiate between preseptal and orbital involvement.
Diagnostic Workup: Diagnosis of preseptal cellulitis is primarily clinical, with imaging studies such as computed tomography (CT) or magnetic resonance imaging (MRI) reserved for cases with atypical presentations or suspected complications. Laboratory investigations may aid in identifying the causative pathogen and guiding antimicrobial therapy.
Management Strategies: Management of preseptal cellulitis involves a multidisciplinary approach, with emphasis on antimicrobial therapy targeting the responsible organism. Empiric antibiotic coverage directed against common pathogens is initiated pending culture results. Surgical intervention may be warranted in cases of abscess formation or refractory infections. Close monitoring for resolution of symptoms and potential complications is essential throughout the treatment course.
Conclusion: Preseptal cellulitis is a frequently encountered entity in ophthalmic practice, necessitating prompt diagnosis and appropriate management to prevent progression to orbital involvement and potential vision-threatening complications. By staying informed about the latest diagnostic and therapeutic modalities, ophthalmologists can effectively manage preseptal cellulitis and optimize patient outcomes.
For further reading and reference:
- American Academy of Ophthalmology (AAO) – Preseptal and Orbital Cellulitis: https://www.aao.org/bcscsnippetdetail.aspx?id=d329d719-0742-41c2-8d8b-3e7a11d724c4
- National Institutes of Health (NIH) – Preseptal Cellulitis: https://www.ncbi.nlm.nih.gov/books/NBK542178/


