Diabetic eye disease, a group of ocular complications resulting from diabetes mellitus, poses a significant threat to vision health worldwide. This article provides a comprehensive examination of diabetic eye disease, covering its pathophysiology, clinical manifestations, diagnostic methods, treatment modalities, and preventive measures.
Introduction: Diabetic eye disease encompasses a spectrum of ocular complications associated with diabetes mellitus, including diabetic retinopathy, diabetic macular edema, cataracts, and glaucoma. Understanding the underlying mechanisms and risk factors for diabetic eye disease is paramount in preventing vision loss and preserving ocular health in individuals with diabetes.
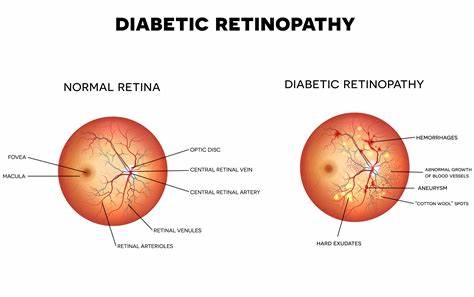
Pathophysiology: The pathophysiology of diabetic eye disease is multifactorial, involving chronic hyperglycemia, oxidative stress, inflammation, and microvascular abnormalities. Prolonged exposure to elevated blood glucose levels leads to damage to the retinal vasculature, resulting in microaneurysms, capillary nonperfusion, and neovascularization, characteristic features of diabetic retinopathy.
Clinical Manifestations: Diabetic eye disease presents with a range of clinical manifestations, including blurred vision, floaters, visual field defects, and progressive vision loss. Diabetic retinopathy may manifest as non-proliferative diabetic retinopathy (NPDR) or proliferative diabetic retinopathy (PDR), with the latter characterized by the growth of abnormal blood vessels on the retina’s surface. Diabetic macular edema (DME) occurs when fluid accumulates in the macula, leading to central vision impairment.
Diagnostic Methods: Diagnosing diabetic eye disease requires a comprehensive ophthalmic evaluation, including visual acuity assessment, dilated fundus examination, and imaging studies. Optical coherence tomography (OCT), fluorescein angiography (FA), and fundus photography are indispensable tools for detecting and monitoring retinal changes associated with diabetic retinopathy and macular edema.
Treatment Modalities: Management of diabetic eye disease aims to prevent disease progression, alleviate symptoms, and preserve visual function. Laser photocoagulation, intravitreal anti-vascular endothelial growth factor (anti-VEGF) injections, and corticosteroid implants are commonly employed to treat diabetic retinopathy and macular edema. Surgical interventions such as vitrectomy may be indicated for advanced cases of proliferative diabetic retinopathy or vitreous hemorrhage.
Preventive Measures: Preventing diabetic eye disease requires a multidisciplinary approach, including optimal glycemic control, blood pressure management, and regular ophthalmic screening. Educating patients about the importance of diabetes management, lifestyle modifications, and adherence to prescribed medications is essential in preventing vision-threatening complications associated with diabetes mellitus.
Conclusion: Diabetic eye disease remains a significant cause of vision impairment and blindness worldwide, particularly among individuals with poorly controlled diabetes. Early detection, timely intervention, and comprehensive management are essential in minimizing the impact of diabetic eye disease on visual function and quality of life. By raising awareness, promoting regular eye examinations, and advocating for integrated diabetes care, we can work towards reducing the global burden of diabetic eye disease and improving outcomes for patients with diabetes.
Links:


