Exploring Posterior Segment Manifestations of HIV-Associated Diseases: A Comprehensive Review
Posterior segment manifestations of HIV-associated diseases encompass a diverse array of ocular findings that reflect the systemic impact of the human immunodeficiency virus (HIV) on the retina, choroid, and optic nerve. This review article aims to provide an in-depth analysis of the posterior segment manifestations seen in individuals with HIV infection, including their pathogenesis, clinical presentations, diagnostic considerations, treatment modalities, and management strategies.
Introduction: The posterior segment of the eye, comprising the retina, choroid, and optic nerve, is susceptible to various complications in individuals living with HIV due to immune dysregulation and opportunistic infections associated with the virus. Understanding the posterior segment manifestations of HIV-associated diseases is crucial for ophthalmologists, as these findings may serve as indicators of systemic HIV progression and immune compromise.
Pathogenesis: The pathogenesis of posterior segment manifestations in HIV-infected individuals involves a complex interplay of viral replication, immune dysfunction, opportunistic infections, and inflammatory responses. HIV-associated posterior segment diseases may result from direct viral invasion, immune reconstitution inflammatory syndrome (IRIS), or secondary infections such as cytomegalovirus (CMV) retinitis, toxoplasmosis, and cryptococcal meningitis.
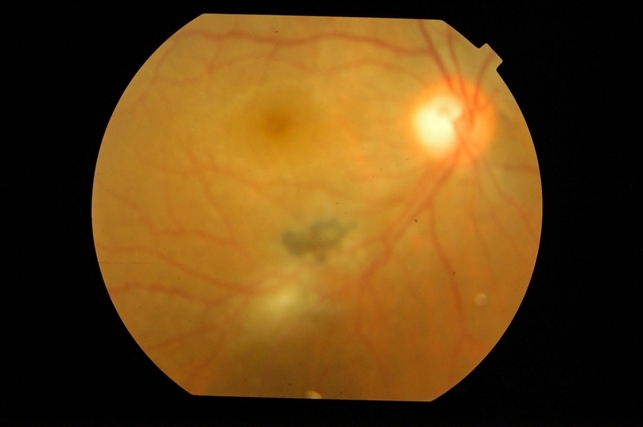
Clinical Presentations: Posterior segment manifestations of HIV-associated diseases encompass a broad spectrum of clinical presentations, including retinitis, chorioretinitis, neuroretinitis, optic neuritis, and macular edema. Patients may present with visual impairment, floaters, scotomas, photopsias, metamorphopsia, and decreased visual acuity, indicative of underlying HIV-related pathology.
Diagnostic Considerations: Diagnosing posterior segment manifestations of HIV-associated diseases requires a comprehensive ophthalmic examination, including dilated funduscopy, optical coherence tomography (OCT), fundus fluorescein angiography (FFA), indocyanine green angiography (ICGA), and ancillary tests such as polymerase chain reaction (PCR) and serologic testing for infectious etiologies. Collaboration with infectious disease specialists and neurologists may be necessary for definitive diagnosis and management.
Treatment Modalities: Management of posterior segment manifestations in HIV-infected individuals involves a multidisciplinary approach, including antiretroviral therapy (ART) to control viral replication, systemic antimicrobial agents for treating opportunistic infections, intravitreal injections of antiviral or anti-inflammatory medications, and laser photocoagulation or vitrectomy for complications such as retinal detachment or vitreous hemorrhage.
Management Strategies: Optimizing visual outcomes and preserving ocular health in HIV-infected individuals with posterior segment manifestations necessitates close collaboration between ophthalmologists, HIV specialists, and other healthcare providers. Regular monitoring, early intervention, and adherence to ART are essential in preventing vision-threatening complications and improving overall patient outcomes.
Conclusion: Posterior segment manifestations of HIV-associated diseases represent a significant source of ocular morbidity and visual impairment in individuals living with HIV. By elucidating the pathogenesis, clinical presentations, diagnostic considerations, treatment modalities, and management strategies associated with these complex ocular conditions, we can enhance our understanding of HIV-related ocular disease and improve patient care.
Links:


