Retinal Artery Occlusion: A Comprehensive Review
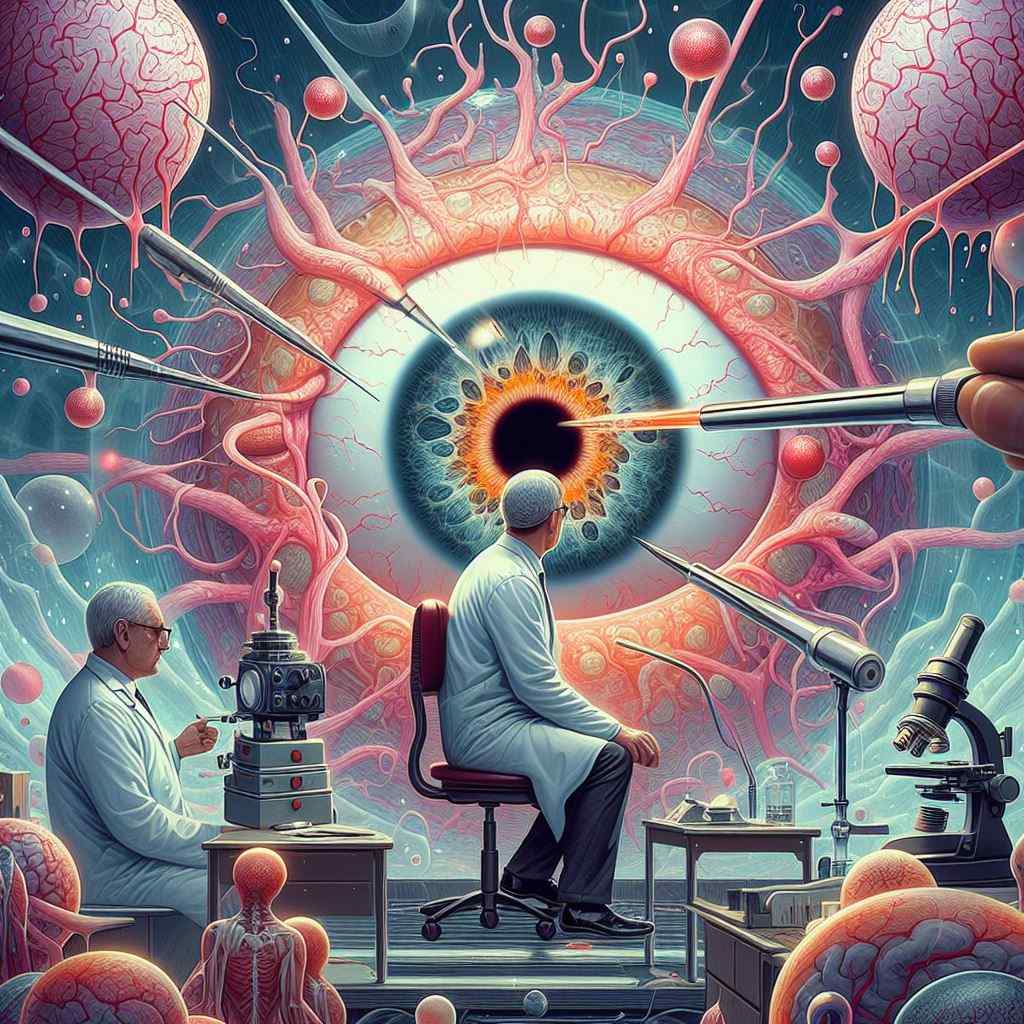
Introduction: Retinal artery occlusion (RAO) encompasses a spectrum of conditions characterized by the obstruction of retinal blood flow, leading to ischemia and potentially irreversible vision loss. This article provides a comprehensive review of three primary types of RAO: Central Retinal Artery Occlusion (CRAO), Branch Retinal Artery Occlusion (BRAO), and Cilioretinal Artery Occlusion (CLRAO), including their etiology, clinical features, diagnostic approaches, management strategies, and prognostic implications.
Central Retinal Artery Occlusion (CRAO): CRAO is a severe form of RAO resulting from the complete obstruction of the central retinal artery, typically at the level of the optic nerve head. Patients with CRAO typically present with sudden, painless, monocular vision loss, often described as a curtain descending over the visual field. Fundus examination may reveal a pale, edematous retina with a cherry-red spot at the fovea. Immediate intervention is essential to preserve vision, with treatment options including ocular massage, anterior chamber paracentesis, and systemic thrombolysis.
Branch Retinal Artery Occlusion (BRAO): BRAO occurs when one of the branches of the central retinal artery becomes occluded, leading to segmental retinal ischemia. Patients with BRAO may experience sudden, painless vision loss corresponding to the affected retinal territory. Fundus examination typically reveals sectoral retinal whitening and the presence of emboli at the site of arterial bifurcation. Management of BRAO involves addressing underlying systemic risk factors and implementing prophylactic measures to prevent recurrence.
Cilioretinal Artery Occlusion (CLRAO): CLRAO involves the occlusion of the cilioretinal artery, a branch of the posterior ciliary artery that supplies the macula. Unlike CRAO and BRAO, CLRAO typically spares central vision due to the preservation of macular perfusion from the unaffected retinal circulation. However, patients may still experience visual field defects corresponding to the affected area of the retina. Management of CLRAO focuses on optimizing macular function and addressing any underlying systemic conditions.
Diagnostic Approaches: Diagnosing RAO requires a comprehensive ophthalmic evaluation, including visual acuity assessment, pupillary examination, intraocular pressure measurement, and detailed fundus examination. Additional diagnostic modalities such as fluorescein angiography (FA), optical coherence tomography (OCT), and visual field testing may be utilized to confirm the diagnosis and assess the extent of retinal ischemia.
Management Strategies: Management of RAO aims to restore retinal perfusion, alleviate ischemic damage, and preserve residual vision. Treatment options include ocular massage, anterior chamber paracentesis, intravenous or intra-arterial thrombolysis, and hyperbaric oxygen therapy. Prompt referral to a multidisciplinary team, including ophthalmologists, neurologists, and vascular specialists, is essential for coordinating comprehensive care and optimizing outcomes.
Prognostic Implications: The prognosis of RAO depends on several factors, including the extent of retinal ischemia, the duration of arterial occlusion, and the presence of associated systemic conditions. Despite aggressive management, RAO may result in permanent visual impairment or even blindness in severe cases. Long-term monitoring and vigilant management of systemic risk factors are essential for preventing recurrence and preserving visual function.
Reference Sites:
- American Academy of Ophthalmology (AAO) – https://www.aao.org/
- National Eye Institute (NEI) – https://www.nei.nih.gov/
- Review of Ophthalmology – https://www.reviewofophthalmology.com/
- Retina Today – https://retinatoday.com/
This comprehensive review provides ophthalmologists with valuable insights into the etiology, clinical features, diagnostic approaches, management strategies, and prognostic implications of retinal artery occlusion, encompassing Central Retinal Artery Occlusion (CRAO), Branch Retinal Artery Occlusion (BRAO), and Cilioretinal Artery Occlusion (CLRAO). By integrating evidence-based practices and leveraging multidisciplinary care, clinicians can effectively manage RAO and optimize visual outcomes for affected patients.


