Understanding Vasoproliferative Retinal Tumor: Insights into Etiology, Diagnosis, and Treatment
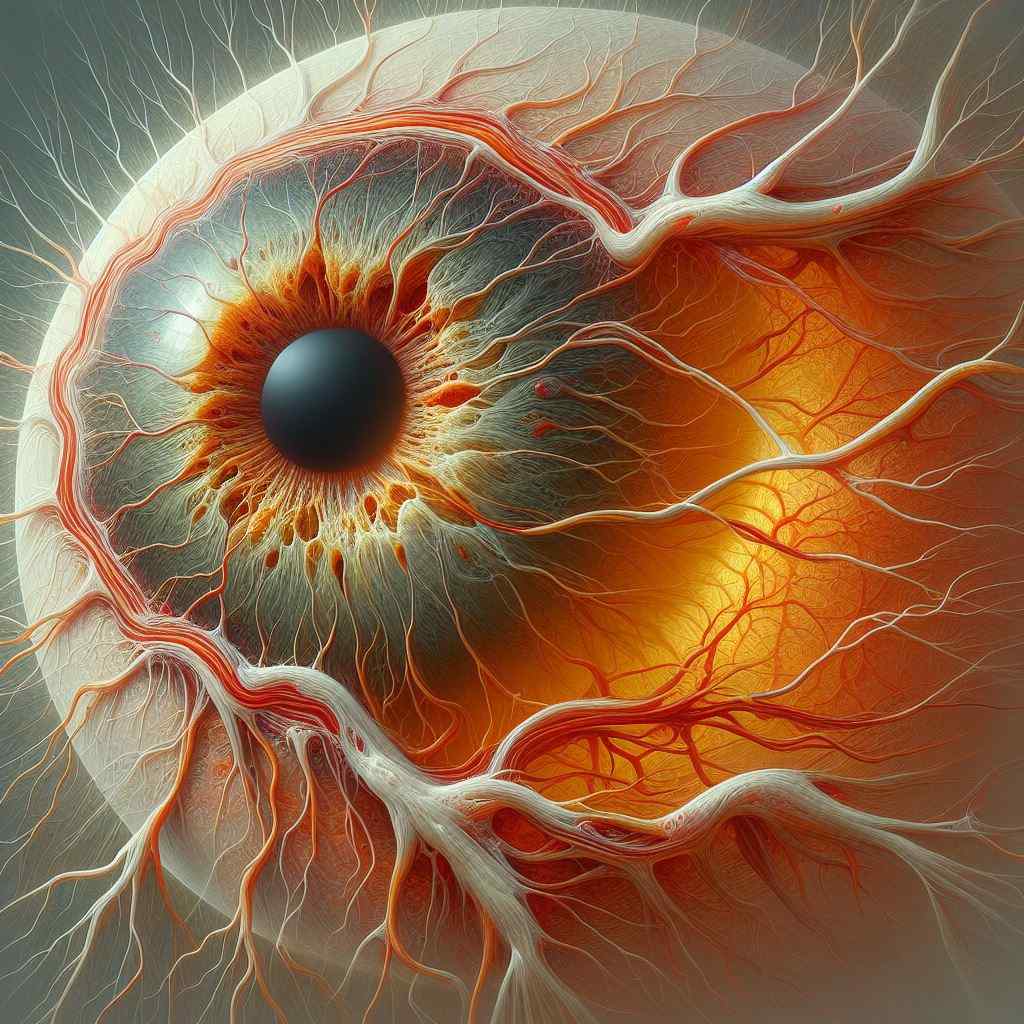
Introduction: Vasoproliferative retinal tumor (VPRT) is a rare, benign intraocular neoplasm originating from the retina or retinal pigment epithelium. This article provides a comprehensive overview of VPRT, including its etiology, clinical features, diagnostic modalities, and treatment options.
Etiology: The exact etiology of VPRT remains unclear, although it is believed to arise from retinal glial cells or the retinal pigment epithelium. Factors such as chronic inflammation, trauma, or genetic predisposition may contribute to its development. VPRTs are typically unilateral and sporadic, although rare cases of bilateral or familial occurrence have been reported.
Clinical Features: Patients with VPRT may present with a variety of symptoms, including decreased visual acuity, visual field defects, floaters, or metamorphopsia. Clinical examination may reveal:
- Presence of a yellowish-white, elevated retinal mass, often located in the peripheral retina.
- Associated features such as retinal exudation, subretinal fluid accumulation, or retinal detachment.
- Angiographic characteristics showing late-phase hyperfluorescence on fluorescein angiography (FA) and hyporeflective areas on optical coherence tomography (OCT).
Diagnostic Modalities: Diagnosis of VPRT relies on a combination of clinical examination and ancillary tests. Key diagnostic modalities include:
- Ophthalmic examination: Dilated fundus examination to visualize the retinal lesion and assess associated findings such as exudation or retinal detachment.
- Fluorescein angiography (FA): To evaluate the vascular characteristics and leakage pattern of the tumor.
- Optical coherence tomography (OCT): Provides detailed cross-sectional imaging of retinal layers and helps assess macular involvement or subretinal fluid.
- Ultrasonography: Useful for detecting the extent of retinal thickening, subretinal fluid, or associated retinal detachment, particularly in cases with poor visualization on fundoscopy.
Treatment Options: Management of VPRT depends on factors such as tumor size, location, and associated complications. Treatment options include:
- Observation: Small, asymptomatic tumors may be monitored closely for any progression or associated complications.
- Laser photocoagulation: Focal laser treatment aimed at inducing tumor regression and reducing associated exudation.
- Cryotherapy: Cryoablation may be considered for larger tumors or those located in proximity to the optic nerve or macula.
- Intravitreal anti-vascular endothelial growth factor (anti-VEGF) agents: In cases with significant exudation or neovascularization, intravitreal injections of anti-VEGF agents may help reduce leakage and improve visual outcomes.
- Surgical intervention: Pars plana vitrectomy with or without tumor resection may be indicated for cases with extensive vitreous hemorrhage, tractional retinal detachment, or persistent exudation refractory to other treatment modalities.
Prognosis: The prognosis of VPRT is generally favorable, with many cases demonstrating stable or regressed tumors and improved visual acuity following treatment. However, vision loss or complications such as retinal detachment may occur in advanced or untreated cases. Long-term follow-up is essential to monitor for tumor recurrence or progression.
Reference Sites:
- American Society of Retina Specialists (ASRS) – https://www.asrs.org/
- Retina Today – https://retinatoday.com/
- PubMed Central (PMC) – [Link to relevant research articles and case studies]
By providing a comprehensive overview of VPRT, this article aims to enhance understanding among healthcare professionals and facilitate optimal management of affected individuals. Continued research efforts are needed to further elucidate the pathogenesis and refine treatment strategies for this rare retinal tumor.


