Exploring White Dot Syndromes: An In-Depth Analysis
Introduction: White dot syndromes (WDS) encompass a group of idiopathic inflammatory conditions characterized by the presence of white or yellowish lesions at the level of the retinal pigment epithelium (RPE) or outer retina. This article provides a comprehensive examination of various white dot syndromes, including their clinical features, differential diagnosis, diagnostic approach, and management strategies.
Clinical Features: White dot syndromes manifest with a range of ocular symptoms and signs, including:
- Decreased Visual Acuity: Patients often present with blurred vision, which may be unilateral or bilateral depending on the extent of retinal involvement.
- Scotomas: Central or paracentral scotomas may develop, affecting visual function and quality of life.
- Photopsia: Some individuals report experiencing flashes of light or photopsias, especially in cases with active inflammation.
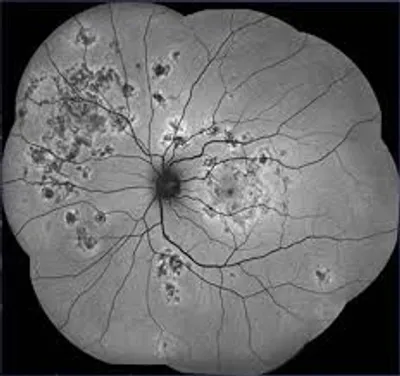
- Fundus Findings: Ophthalmoscopic examination reveals characteristic white or yellowish lesions at the level of the RPE, varying in size, shape, and distribution. Lesions may be focal or multifocal and can involve the posterior pole, midperiphery, or peripheral retina.
Differential Diagnosis: The differential diagnosis of white dot syndromes includes various inflammatory, infectious, neoplastic, and degenerative conditions:
- Acute Retinal Necrosis (ARN): A viral retinitis characterized by necrotizing retinitis and occlusive vasculitis, typically caused by herpes simplex virus or varicella-zoster virus.
- Multifocal Choroiditis (MFC): Inflammatory disorder involving the choroid and RPE, presenting with multiple discrete lesions and associated vitritis.
- Birdshot Chorioretinopathy: Chronic bilateral posterior uveitis characterized by creamy white choroidal lesions and vitreous inflammation.
- Serpiginous Choroidopathy: Progressive inflammatory chorioretinopathy characterized by geographic areas of choroidal and RPE involvement.
- Acute Macular Neuroretinopathy (AMN): Rare condition characterized by paracentral scotomas and reddish-brown parafoveal lesions on fundus examination.
Diagnostic Approach: The diagnosis of white dot syndromes involves a combination of clinical evaluation, imaging studies, and laboratory investigations:
- Ophthalmic Examination: Detailed assessment of visual acuity, intraocular pressure, anterior segment evaluation, and dilated fundus examination.
- Imaging Modalities: Optical coherence tomography (OCT), fundus autofluorescence (FAF), fluorescein angiography (FA), and indocyanine green angiography (ICGA) to assess retinal and choroidal architecture, RPE integrity, and vascular perfusion.
- Laboratory Tests: Serologic testing for infectious etiologies (e.g., herpesviruses, syphilis), HLA typing, and genetic testing in selected cases to identify underlying predisposing factors.
Management Strategies: Treatment of white dot syndromes aims to suppress ocular inflammation, preserve visual function, and prevent disease progression:
- Corticosteroids: Systemic corticosteroids (e.g., prednisone) are often used as first-line therapy to induce remission of inflammation. Topical or periocular corticosteroids may be adjunctively employed for anterior segment involvement.
- Immunomodulatory Agents: In cases of steroid dependence or refractory disease, immunomodulatory agents such as methotrexate, azathioprine, mycophenolate mofetil, or biologic agents (e.g., adalimumab) may be considered to achieve disease control and reduce the risk of relapse.
Reference Sites:
- American Academy of Ophthalmology (AAO) – https://www.aao.org/
- Retina Society – https://www.retinasociety.org/
- PubMed Central (PMC) – [Link to relevant research articles and clinical guidelines]
By providing an in-depth analysis of white dot syndromes, this article aims to enhance understanding among ophthalmologists and facilitate accurate diagnosis and optimal management of these complex inflammatory conditions. Continued research efforts are crucial to elucidate disease mechanisms, refine diagnostic criteria, and develop targeted therapies for improved patient outcomes.


