Acute Anterior Uveitis: Insights into Pathogenesis, Diagnosis, and Management
Abstract: Acute anterior uveitis (AAU) represents a common and potentially sight-threatening inflammatory condition of the eye. This article provides a comprehensive review of AAU, encompassing its epidemiology, etiology, clinical features, diagnostic modalities, treatment strategies, and recent advancements. By enhancing our understanding of AAU, ophthalmologists can optimize patient care and improve visual outcomes.
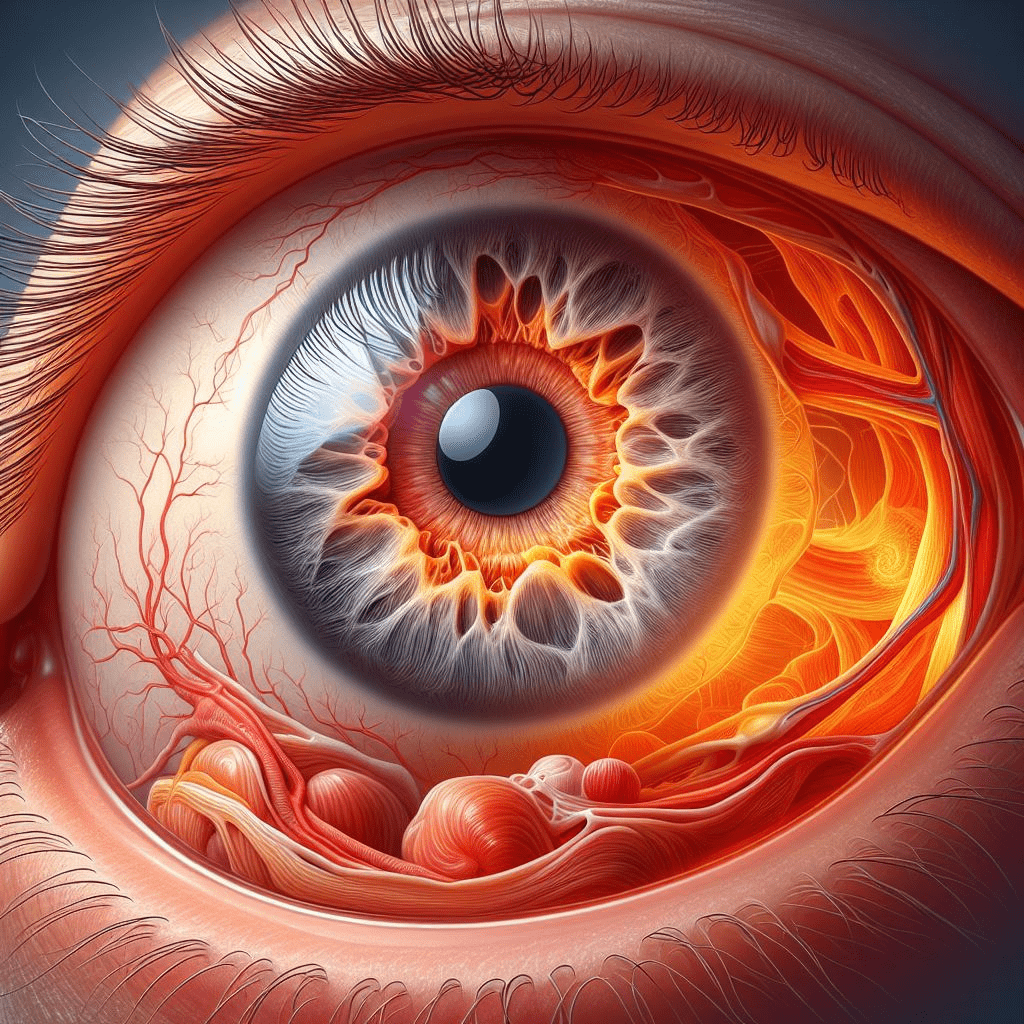
Introduction: Acute anterior uveitis (AAU), also known as iritis, is characterized by inflammation of the anterior segment of the uvea, including the iris and ciliary body. It typically presents with sudden-onset ocular pain, photophobia, blurred vision, and redness, necessitating prompt evaluation and management to prevent complications.
Epidemiology: AAU accounts for a significant proportion of uveitis cases, with an estimated annual incidence of 8 to 15 cases per 100,000 individuals. It affects individuals of all ages, but peaks in incidence occur between the second and fourth decades of life. There is a predilection for certain populations, including those with HLA-B27 genetic predisposition.
Etiology and Pathogenesis: While the exact cause of AAU remains elusive, it is believed to involve a complex interplay of genetic, immunologic, and environmental factors. Associations with HLA-B27, infections (e.g., HLA-B27-associated seronegative spondyloarthropathies), and systemic inflammatory conditions (e.g., ankylosing spondylitis, inflammatory bowel disease) underscore the heterogeneous nature of AAU etiology.
Clinical Features: The hallmark clinical features of AAU include anterior chamber inflammation (cells and flare), iris synechiae formation, and posterior synechiae in severe cases. Slit-lamp examination is crucial for evaluating anterior segment inflammation, assessing for complications such as hypopyon, and monitoring treatment response.
Diagnostic Modalities: Ancillary tests such as anterior segment optical coherence tomography (AS-OCT) and ultrasound biomicroscopy (UBM) can provide detailed visualization of anterior segment structures and aid in the assessment of disease severity and complications. Laboratory investigations, including HLA-B27 testing and serologic studies, may be warranted to identify underlying systemic associations.
Treatment Strategies: The management of AAU is multifaceted and tailored to the severity of inflammation, underlying etiology, and patient-specific factors. Topical corticosteroids remain the mainstay of treatment for mild to moderate cases, while systemic immunomodulatory agents (e.g., oral corticosteroids, disease-modifying anti-rheumatic drugs) may be indicated for refractory or recurrent disease.
Recent Advances: Emerging therapeutic modalities such as biologic agents targeting pro-inflammatory cytokines (e.g., tumor necrosis factor-alpha inhibitors) hold promise for improving outcomes in AAU by providing targeted immunomodulation while minimizing systemic side effects. Additionally, advances in imaging technologies and molecular diagnostics offer new avenues for early diagnosis and personalized treatment approaches.
Conclusion: Acute anterior uveitis poses diagnostic and therapeutic challenges to ophthalmologists, requiring a multidisciplinary approach for optimal management. By leveraging the latest innovations in diagnostic modalities and treatment strategies, clinicians can effectively control inflammation, preserve visual function, and enhance patient quality of life.
For further reading and reference:
- American Academy of Ophthalmology – Uveitis: https://www.aao.org/topic/uveitis
- Uveitis.org – Patient Information: https://uveitis.org/patient


