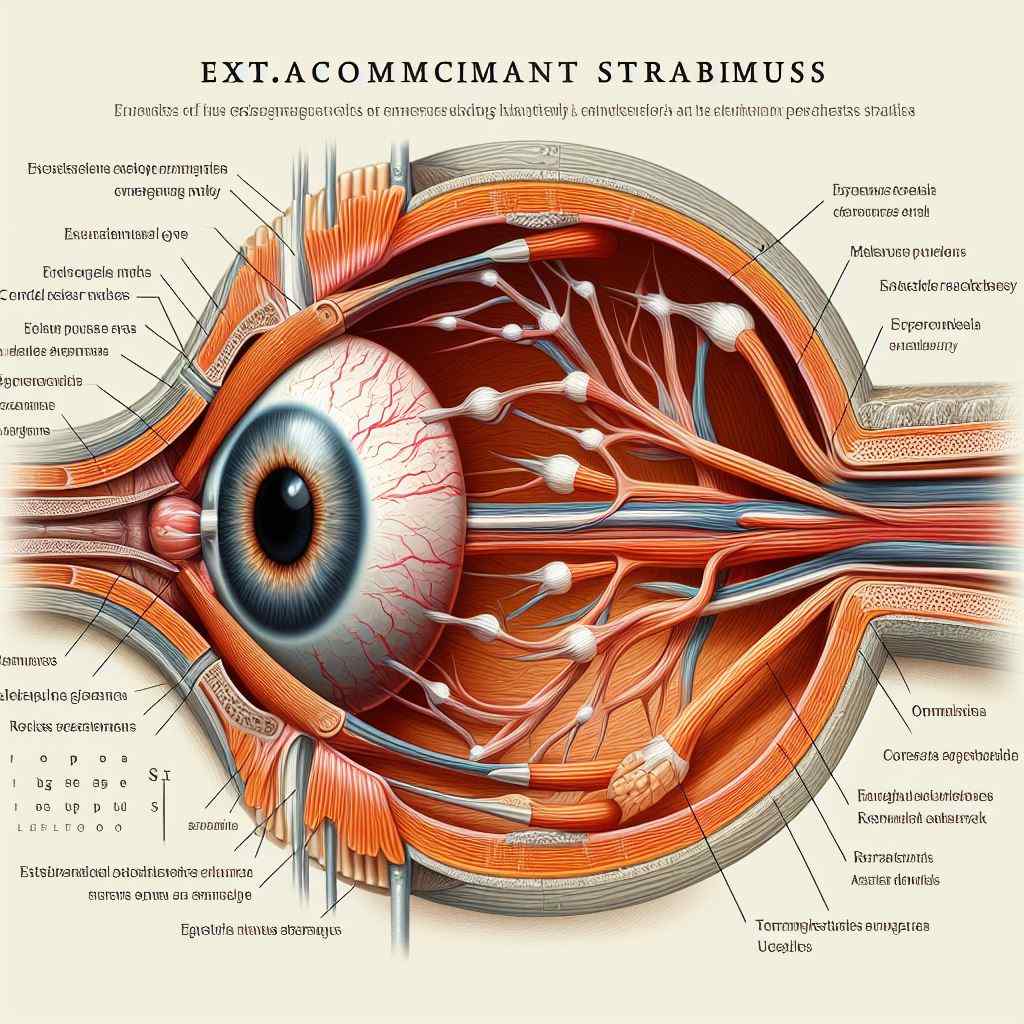
Exploring Incomitant Strabismus
Introduction: Incomitant strabismus refers to a type of ocular misalignment characterized by variations in the angle of deviation between different positions of gaze. Unlike concomitant strabismus, where the deviation remains consistent across all directions of gaze, incomitant strabismus exhibits a variable deviation that may change with changes in fixation or gaze direction. This article provides an in-depth examination of incomitant strabismus, including its clinical features, etiology, diagnosis, management, and potential complications.
Clinical Features:
- Variable Deviation: Incomitant strabismus manifests as an ocular misalignment that varies in magnitude depending on the direction of gaze.
- Paralytic vs. Non-Paralytic: Incomitant strabismus can be categorized as paralytic, resulting from muscle paralysis or paresis, or non-paralytic, where the deviation is not related to muscle dysfunction.
- Diplopia: Individuals with incomitant strabismus may experience diplopia (double vision) due to the misalignment of the eyes in different gaze positions.
- Compensatory Head Postures: Some patients may adopt compensatory head postures to minimize diplopia and maintain binocular fusion.
Etiology:
- Muscular Dysfunction: Incomitant strabismus may arise from muscular dysfunction, such as cranial nerve palsy (e.g., third, fourth, or sixth nerve palsy) or restrictive strabismus caused by orbital or extraocular muscle fibrosis.
- Mechanical Factors: Mechanical factors, including orbital trauma, thyroid eye disease, or orbital tumors, can lead to restrictive strabismus by limiting the movement of the affected eye.
- Neurological Disorders: Neurological conditions affecting the brainstem or cranial nerves can disrupt the neural control of eye movements, resulting in incomitant strabismus.
Diagnosis:
- Clinical Evaluation: A thorough clinical evaluation, including assessment of ocular motility, cover testing, and evaluation of binocular vision, is essential to diagnose incomitant strabismus accurately.
- Neuroimaging: Neuroimaging studies, such as magnetic resonance imaging (MRI) or computed tomography (CT) scans, may be indicated to evaluate for underlying structural abnormalities or lesions affecting the ocular motor system.
- Electrophysiological Testing: Electrophysiological tests, including electrooculography (EOG) or electromyography (EMG), may be employed to assess the function of extraocular muscles and cranial nerves.
Management:
- Treatment of Underlying Cause: Management of incomitant strabismus involves addressing the underlying etiology, which may include medical or surgical interventions targeted at correcting muscle dysfunction, relieving mechanical restrictions, or treating neurological conditions.
- Prism Lenses: Prism lenses may be prescribed to alleviate diplopia and improve binocular vision by optically shifting the image to a non-foveal area of the retina.
- Strabismus Surgery: Surgical correction of incomitant strabismus aims to realign the eyes by adjusting the tension or position of extraocular muscles or addressing mechanical restrictions through procedures such as muscle recession, resection, or transposition.
- Vision Therapy: Vision therapy may complement surgical or optical interventions by improving ocular motility, binocular fusion, and visual processing skills through targeted exercises and activities.
Complications:
- Persistent Diplopia: Despite treatment, some individuals may continue to experience diplopia, particularly if the underlying cause of incomitant strabismus cannot be fully corrected.
- Decreased Quality of Life: Incomitant strabismus and associated diplopia can significantly impact an individual’s quality of life, leading to functional limitations and psychological distress.
Conclusion: Incomitant strabismus presents a diagnostic and management challenge due to its variable deviation and diverse etiology. By employing a multidisciplinary approach that integrates clinical evaluation, neuroimaging, and targeted interventions, ophthalmologists can effectively diagnose and manage incomitant strabismus, optimizing visual outcomes and enhancing patient quality of life.
Reference Sites:
- American Association for Pediatric Ophthalmology and Strabismus (AAPOS) – https://www.aapos.org/
- American Academy of Ophthalmology (AAO) – https://www.aao.org/
- PubMed Central (PMC) – [Link to relevant research articles and clinical guidelines]
This article aims to deepen understanding of the clinical features, etiology, diagnosis, management, and potential complications of incomitant strabismus, fostering improved care and outcomes for individuals with this condition. Continued research and collaboration within the ophthalmic community are essential for advancing knowledge and refining treatment strategies for incomitant strabismus.


