Exploring Uveitis with Juvenile Idiopathic Arthritis: A Comprehensive Overview
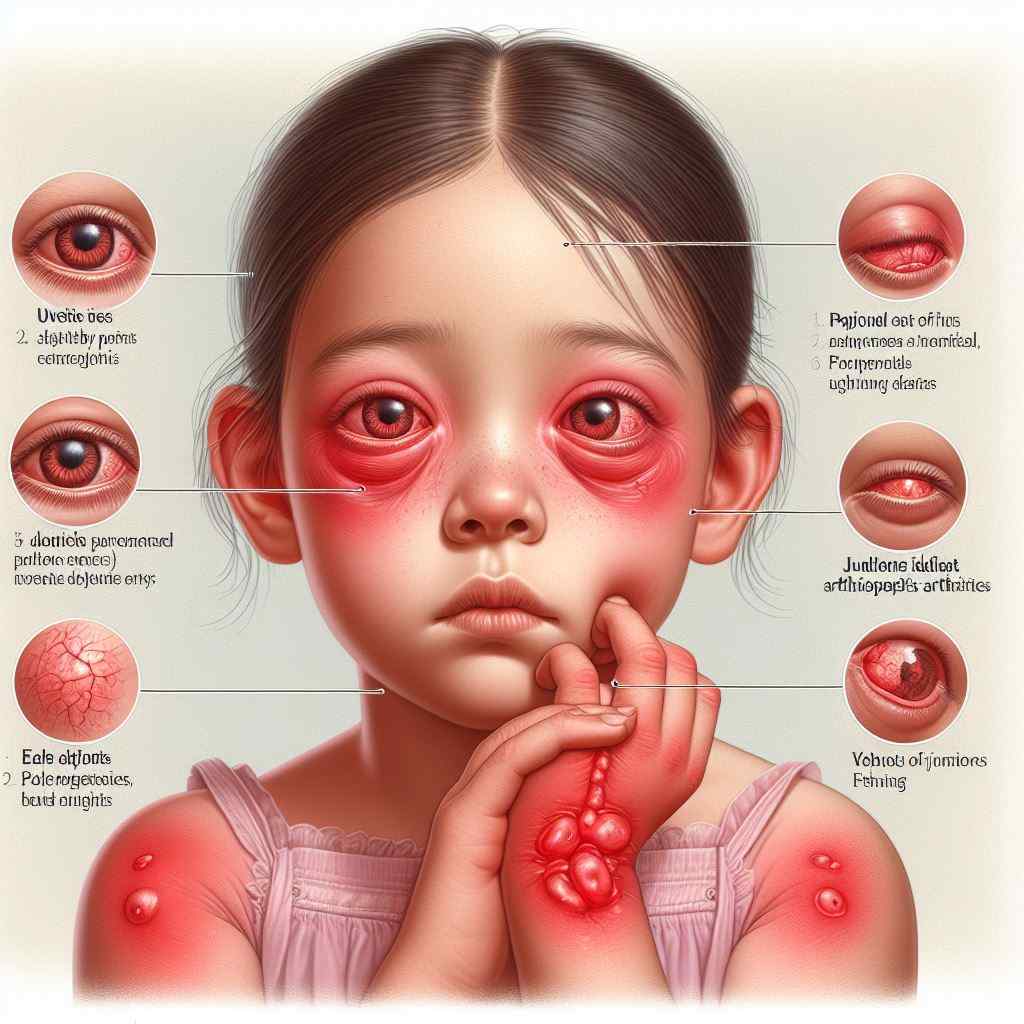
Introduction: Uveitis associated with juvenile idiopathic arthritis (JIA) is a significant ocular complication characterized by intraocular inflammation in children with arthritis of unknown cause. This article provides a comprehensive exploration of uveitis in the context of JIA, including its epidemiology, pathogenesis, clinical features, diagnostic approaches, treatment strategies, and associated challenges.
Epidemiology: Uveitis is a common extra-articular manifestation of JIA, occurring in approximately 10-20% of children with the condition. It typically presents within the first few years after JIA onset and can lead to significant visual morbidity if not promptly diagnosed and managed. The risk of uveitis varies based on JIA subtype, with the highest prevalence observed in oligoarticular and extended oligoarticular JIA.
Pathogenesis: The exact pathogenesis of uveitis in JIA remains incompletely understood but is thought to involve complex interactions between genetic predisposition, dysregulated immune responses, and environmental factors. Autoimmune mechanisms, including molecular mimicry and aberrant T-cell activation, may play a role in initiating and perpetuating intraocular inflammation.
Clinical Features: Uveitis in JIA often presents insidiously and asymptomatically, making early detection challenging. Common clinical features include:
- Anterior chamber inflammation (anterior uveitis) characterized by anterior chamber cells and flare, posterior synechiae, and keratic precipitates.
- Complications such as cataracts, glaucoma, band keratopathy, and macular edema may develop if inflammation is left untreated.
- Chronic, recurrent course with periods of quiescence and exacerbation, necessitating long-term monitoring and management.
Diagnostic Approaches: Diagnosis of uveitis in JIA relies on a combination of:
- Thorough ophthalmic examination, including slit-lamp biomicroscopy and dilated fundus examination to assess intraocular inflammation and associated complications.
- Ancillary tests such as optical coherence tomography (OCT), fluorescein angiography (FA), and ultrasonography to evaluate retinal and choroidal involvement.
- Systemic evaluation by a pediatric rheumatologist to confirm the diagnosis of JIA and assess disease activity and severity.
Treatment Strategies: Management of uveitis in JIA aims to achieve and maintain disease remission while minimizing ocular complications and preserving vision. Treatment modalities include:
- Topical corticosteroids as first-line therapy for anterior uveitis, with periocular or intraocular corticosteroid injections reserved for more severe cases.
- Systemic immunomodulatory agents such as methotrexate, adalimumab, or infliximab for refractory or sight-threatening uveitis.
- Ongoing ophthalmic monitoring and adjustment of treatment based on disease activity and response.
Associated Challenges: Uveitis in JIA poses several challenges, including:
- Risk of vision loss and ocular complications despite aggressive treatment.
- Adverse effects of systemic immunosuppression, including increased susceptibility to infections and malignancies.
- Need for multidisciplinary collaboration between ophthalmologists, pediatric rheumatologists, and other healthcare providers to optimize patient care.
Reference Sites:
- American College of Rheumatology (ACR) – https://www.rheumatology.org/
- American Uveitis Society (AUS) – https://uveitissociety.org/
- Childhood Arthritis and Rheumatology Research Alliance (CARRA) – [Link to relevant research articles and resources]
By providing a comprehensive overview of uveitis in the context of JIA, this article aims to enhance awareness among healthcare professionals and improve the management and outcomes of affected children. Continued research efforts are essential for advancing our understanding of the pathogenesis and optimal treatment strategies for this challenging condition.