Pioneering Vision Restoration: A Deep Dive into Penetrating Keratoplasty
Abstract: Penetrating keratoplasty (PK) stands as a pioneering surgical procedure for the restoration of vision in patients with various corneal pathologies. This article delves into the intricacies of PK, exploring its historical evolution, surgical techniques, postoperative care, and contemporary advancements.
Introduction: Penetrating keratoplasty (PK), also known as full-thickness corneal transplantation, has been a cornerstone in ophthalmic surgery since its inception. Originally developed to address corneal opacities, PK has evolved to encompass a broad spectrum of indications, ranging from keratoconus and corneal dystrophies to corneal scars and infections.
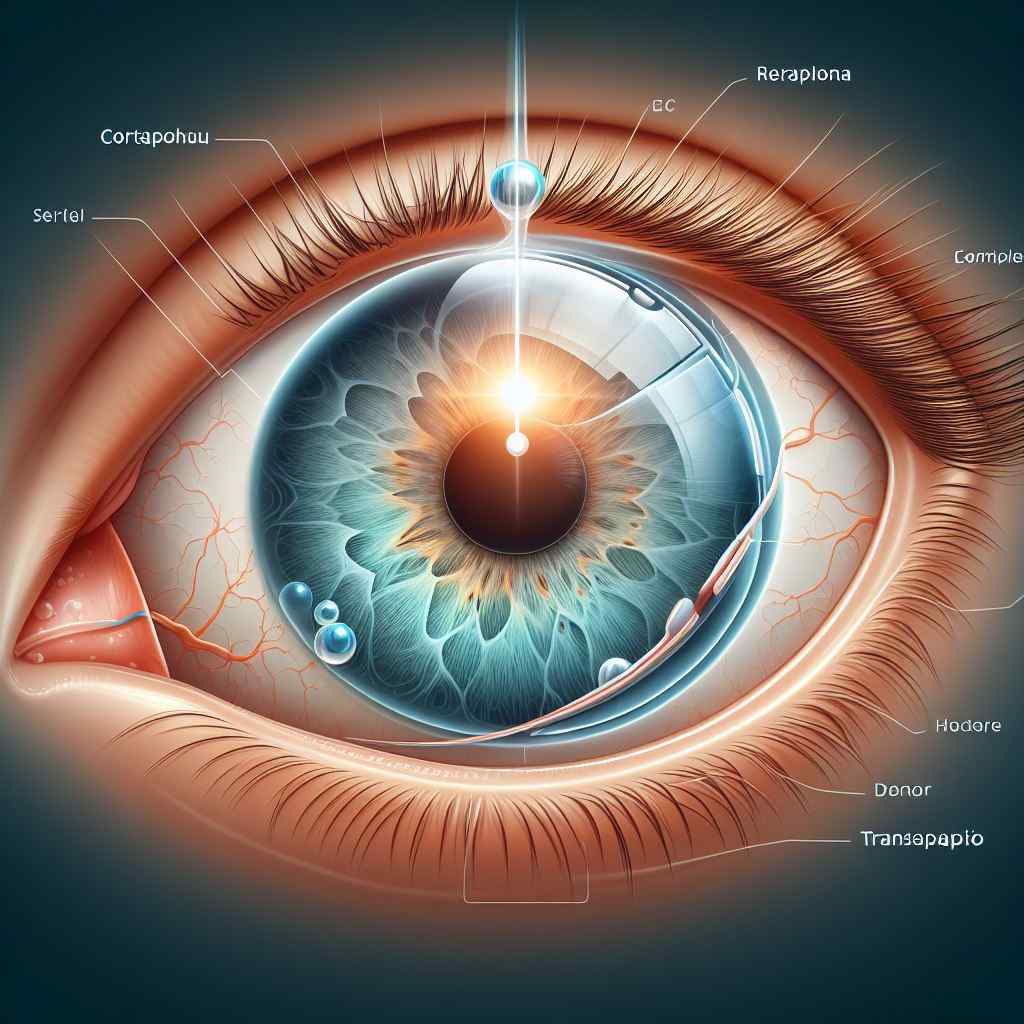
Surgical Technique: PK involves the removal of the recipient’s diseased cornea and replacement with a donor corneal graft. The procedure begins with trephination of the recipient and donor corneas, followed by suturing of the donor graft onto the recipient bed using either interrupted or continuous sutures. Advanced techniques such as femtosecond laser-assisted PK have enhanced precision and outcomes in PK surgeries. (Source: American Academy of Ophthalmology – Penetrating Keratoplasty)
Postoperative Care and Complications: Post-PK care focuses on minimizing graft rejection, managing intraocular pressure, and promoting wound healing. Common complications include graft rejection, graft failure, astigmatism, and glaucoma. Close monitoring and prompt intervention are crucial for optimizing visual outcomes and graft survival rates.
Indications and Patient Selection: PK is indicated for a wide range of corneal disorders, including keratoconus, corneal scars, corneal dystrophies, and corneal degenerations. Patient selection criteria consider factors such as corneal thickness, visual potential, anterior chamber depth, and systemic comorbidities, ensuring optimal outcomes and graft survival.
Outcomes and Prognosis: PK achieves favorable visual outcomes and graft survival rates, particularly in cases of corneal scarring and endothelial dysfunction. Long-term graft survival depends on various factors, including the presence of preexisting ocular conditions, the occurrence of graft rejection, and adherence to postoperative care regimens. (Source: Journal of Ophthalmic Surgery and Research – Penetrating Keratoplasty Outcomes)
Emerging Trends and Future Directions: Emerging trends in PK include the use of preloaded donor tissue, selective suture techniques, and lamellar dissection methods. Future directions focus on enhancing graft survival rates, reducing surgical complexities, and exploring alternative approaches such as Descemet’s stripping automated endothelial keratoplasty (DSAEK) and Descemet’s membrane endothelial keratoplasty (DMEK) for endothelial dysfunction.
Conclusion: In conclusion, penetrating keratoplasty remains a cornerstone in corneal transplantation, offering hope and restoration of vision to patients with various corneal disorders. By embracing technological advancements, refining surgical techniques, and optimizing patient selection criteria, we can continue to improve outcomes and enhance quality of life for individuals undergoing PK surgery.


