Understanding Pterygium: A Comprehensive Guide to Diagnosis and Management
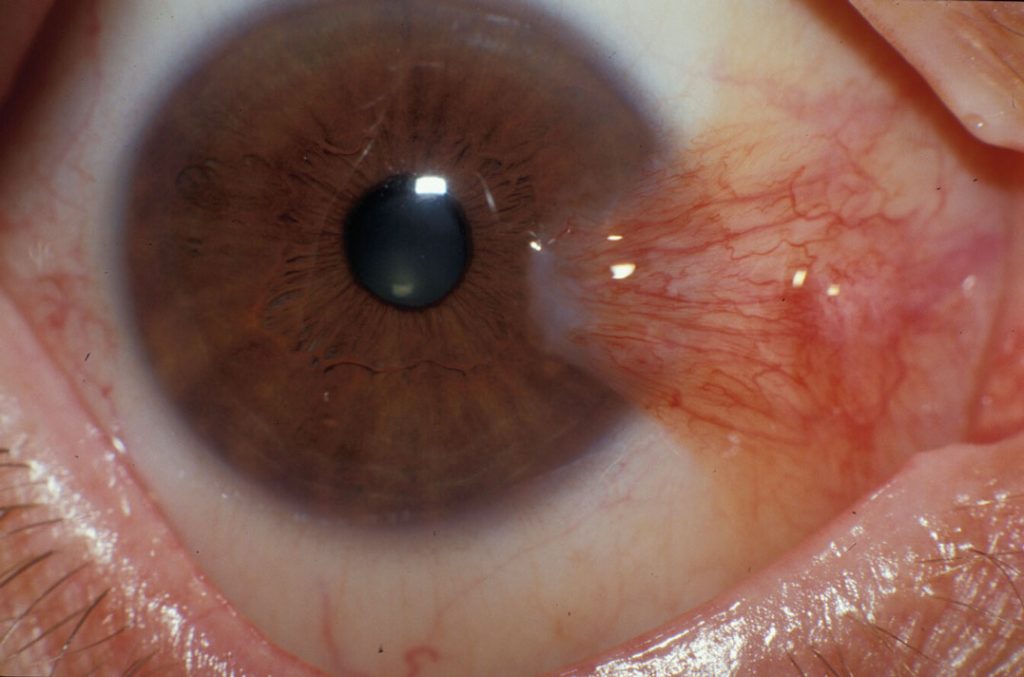
Abstract: Pterygium is a common ocular surface disorder characterized by a fleshy growth of conjunctival tissue onto the cornea. This article provides an in-depth exploration of pterygium, encompassing its etiology, clinical presentation, diagnostic considerations, treatment options, and potential complications. By enhancing understanding of this condition, clinicians can effectively assess and manage patients with pterygium, optimizing visual outcomes and reducing the risk of recurrence.
Introduction: Pterygium is a prevalent ocular condition characterized by the proliferation of fibrovascular tissue from the conjunctiva onto the cornea. While typically benign, pterygium can cause significant discomfort, visual disturbances, and cosmetic concerns. Understanding the underlying pathophysiology and risk factors is essential for guiding appropriate management strategies.
Etiology and Risk Factors: The exact etiology of pterygium remains unclear, but chronic exposure to ultraviolet (UV) radiation, environmental factors (such as dust and wind), and genetic predisposition are believed to play key roles in its development. Individuals residing in sunny, equatorial regions and those with outdoor occupations are at higher risk of developing pterygium.
Clinical Presentation: Pterygium typically presents as a triangular, wing-shaped growth extending from the nasal or temporal conjunctiva onto the cornea. Common symptoms include ocular irritation, foreign body sensation, tearing, and blurred vision. Clinically, pterygium can vary in size, vascularity, and degree of inflammation, with more advanced cases potentially leading to corneal astigmatism and visual impairment.
Diagnostic Considerations: Diagnosing pterygium is primarily based on clinical examination, including slit-lamp biomicroscopy and assessment of lesion characteristics. Differential diagnosis may include other ocular surface conditions such as pinguecula, nodular episcleritis, and ocular surface squamous neoplasia (OSSN). Ancillary tests such as anterior segment photography and optical coherence tomography (OCT) may aid in lesion evaluation and surgical planning.
Treatment Options: Management of pterygium varies based on the severity of symptoms, extent of corneal involvement, and risk of recurrence. Non-surgical interventions, including lubricating eye drops, topical corticosteroids, and UV-protective eyewear, may provide symptomatic relief and prevent lesion progression in mild cases. Surgical excision with conjunctival autografting or amniotic membrane transplantation is often indicated for visually significant or cosmetically bothersome pterygia, aiming to restore ocular surface integrity and minimize recurrence rates.
Potential Complications: Complications associated with pterygium surgery include recurrence, induced astigmatism, dry eye syndrome, and graft-related complications. Close postoperative monitoring and appropriate management of these complications are essential for achieving favorable visual outcomes and patient satisfaction.
Conclusion: Pterygium represents a common ocular surface disorder with significant implications for patient comfort and visual function. By adopting a multidisciplinary approach encompassing prevention, early detection, and tailored management strategies, clinicians can effectively address the diverse needs of patients with pterygium, optimizing ocular health and quality of life. Ongoing research into novel treatment modalities and preventive measures holds promise for further improving outcomes in this challenging condition.