Understanding Retinal Vein Occlusion (RVO): A Comprehensive Review
Introduction: Retinal vein occlusion (RVO) encompasses a spectrum of vascular disorders characterized by the obstruction of retinal veins, leading to impaired blood flow, retinal ischemia, and various sight-threatening complications. This article provides an in-depth analysis of different types of RVO, including central retinal vein occlusion (CRVO), branch retinal vein occlusion (BRVO), and hemicentral retinal vein occlusion (HRVO), focusing on their etiology, clinical manifestations, diagnostic approaches, management strategies, and prognostic considerations.
Etiology: RVO can occur due to various factors, including:
- Arteriosclerosis and vascular diseases (e.g., hypertension, diabetes mellitus)
- Hypercoagulable states and thromboembolic disorders
- Structural abnormalities or compression of retinal veins
- Inflammatory conditions (e.g., uveitis, systemic vasculitis)
- Systemic conditions (e.g., hyperlipidemia, autoimmune diseases)
Clinical Manifestations: The clinical presentation of RVO depends on the type and location of the occlusion, with common features such as:
- Sudden onset or gradual blurring of vision
- Retinal hemorrhages (flame-shaped or dot/blot hemorrhages)
- Retinal edema (macular or peripheral)
- Cotton-wool spots and intraretinal exudates
- Optic disc swelling (papilledema or optic disc edema)
- Macular ischemia and neovascularization (in severe cases)
Diagnostic Approaches: Diagnosing RVO involves a comprehensive ophthalmic evaluation and diagnostic tests, including:
- Fundus examination to assess retinal vascular changes and associated findings
- Optical coherence tomography (OCT) to evaluate macular thickness and morphology
- Fluorescein angiography (FA) to visualize retinal vascular perfusion and leakage
- Optical coherence tomography angiography (OCTA) for non-invasive imaging of retinal vasculature
- Laboratory investigations to identify underlying systemic or hematologic abnormalities
Management Strategies: Management of RVO aims to alleviate symptoms, reduce macular edema, prevent complications, and preserve vision. Treatment modalities may include:
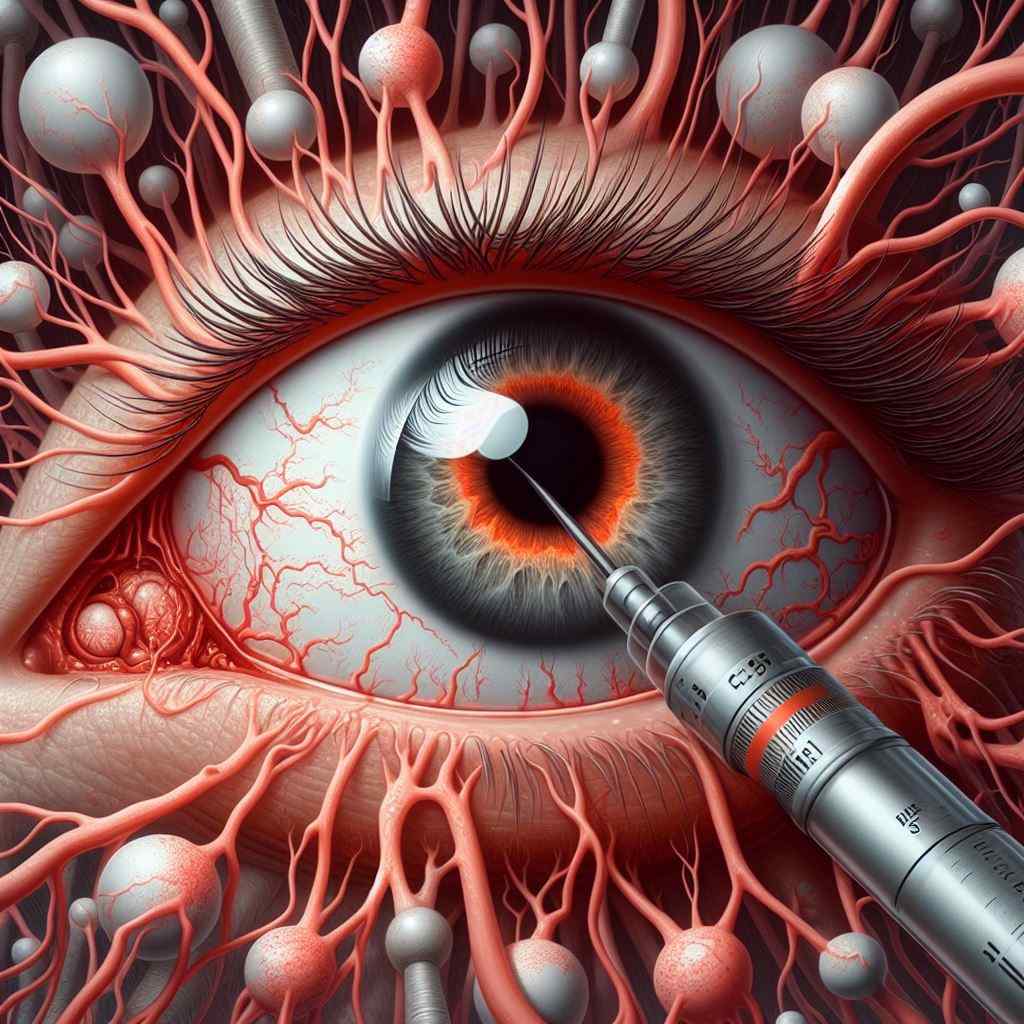
- Intravitreal anti-VEGF injections (e.g., ranibizumab, aflibercept) for macular edema and neovascularization
- Intravitreal corticosteroid injections (e.g., triamcinolone acetonide) for refractory macular edema
- Laser photocoagulation or panretinal photocoagulation (PRP) for ischemic and neovascular complications
- Systemic anticoagulants or antiplatelet agents for selected cases with underlying thromboembolic risk factors
- Surgical interventions (e.g., vitrectomy) for severe vitreous hemorrhage or tractional complications
Prognostic Considerations: The prognosis of RVO depends on various factors, including the extent of retinal ischemia, presence of macular edema, response to treatment, and development of complications such as neovascularization and retinal detachment. Early diagnosis, timely intervention, and close monitoring are crucial for optimizing visual outcomes and preventing irreversible vision loss.
Reference Sites:
- American Society of Retina Specialists (ASRS) – https://www.asrs.org/
- Retina Society – https://www.retinasociety.org/
- Royal College of Ophthalmologists (RCOphth) – https://www.rcophth.ac.uk/
- National Eye Institute (NEI) – https://www.nei.nih.gov/
This comprehensive review aims to enhance the understanding of RVO among ophthalmologists, providing valuable insights into its pathogenesis, clinical features, diagnostic approaches, management options, and prognostic implications. By integrating evidence-based practices and individualized treatment strategies, clinicians can effectively address the challenges posed by RVO and optimize visual outcomes for affected patients.


