Unraveling Ocular Hypertension: Mechanisms, Evaluation, Management, and Recent Innovations
Abstract: Ocular hypertension (OHT) presents a clinical conundrum in ophthalmology, characterized by elevated intraocular pressure (IOP) without evidence of glaucomatous optic neuropathy or visual field defects. This article provides a comprehensive review of OHT, exploring its underlying mechanisms, diagnostic criteria, management strategies, and recent advancements. By delving into the intricacies of OHT, ophthalmologists can refine their approach to patient care and optimize outcomes in this challenging condition.
Introduction: Ocular hypertension represents a significant risk factor for the development of glaucoma, yet not all individuals with elevated IOP progress to glaucomatous optic neuropathy. Understanding the pathophysiology and risk factors associated with OHT is essential for accurate diagnosis and appropriate management.
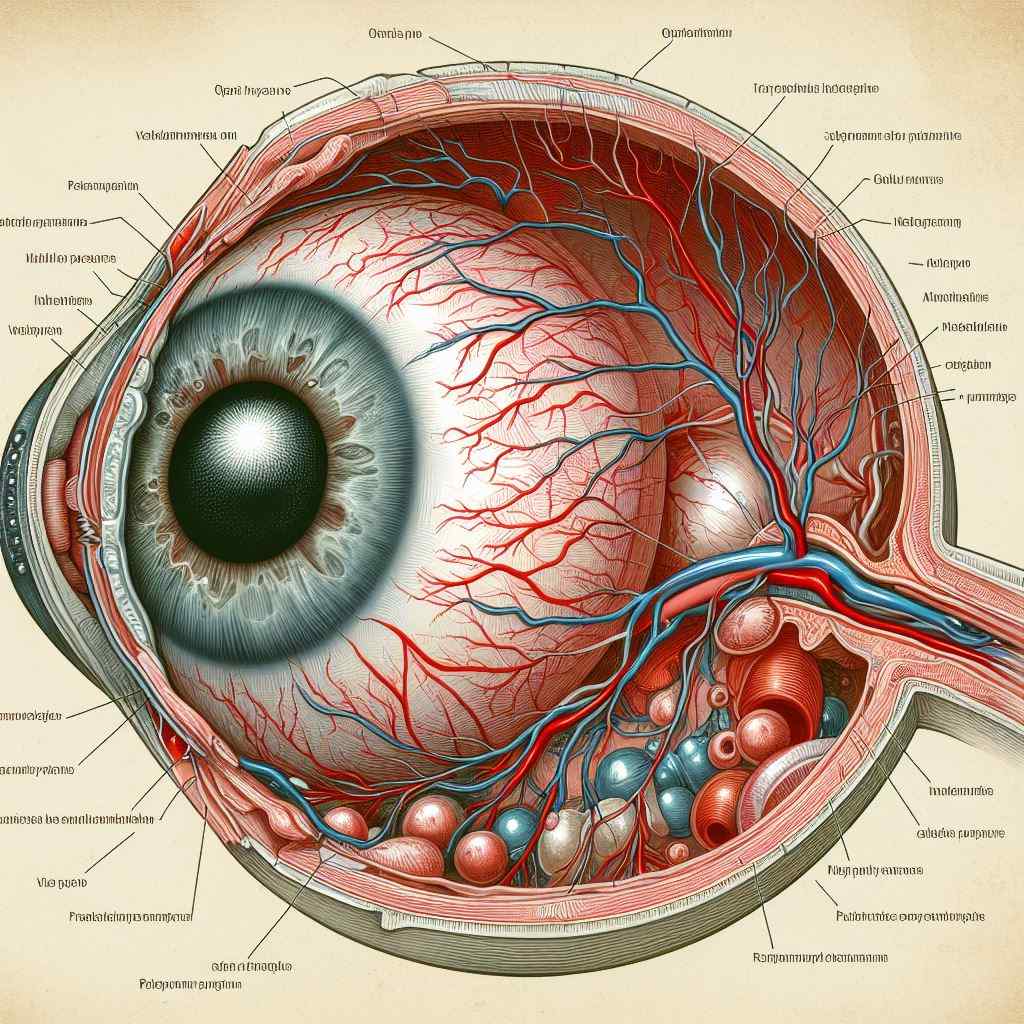
Mechanisms: The pathogenesis of OHT involves disturbances in aqueous humor dynamics, including increased production, decreased outflow facility, or a combination of both factors. Structural abnormalities such as increased central corneal thickness or alterations in trabecular meshwork morphology may also contribute to elevated IOP in OHT.
Diagnostic Criteria: Diagnosis of OHT relies on accurate measurement of IOP and comprehensive evaluation to rule out glaucomatous optic neuropathy or visual field defects. Additional diagnostic tests such as optic nerve imaging with optical coherence tomography (OCT) and visual field testing may aid in identifying early signs of glaucomatous damage.
Management Strategies: Management of OHT aims to reduce the risk of progression to glaucoma while minimizing unnecessary treatment and patient anxiety. Treatment modalities may include regular monitoring of IOP, lifestyle modifications such as smoking cessation and regular exercise, and consideration of pharmacological interventions to lower IOP in high-risk individuals.
Recent Advances: Recent innovations in OHT management focus on improving risk stratification, enhancing diagnostic accuracy, and refining treatment algorithms. Advancements such as artificial intelligence-based algorithms for glaucoma risk prediction and wearable IOP monitoring devices offer potential benefits in identifying individuals at highest risk of progression to glaucoma and optimizing treatment strategies accordingly.
Conclusion: Ocular hypertension represents a complex clinical entity in ophthalmology, requiring a nuanced approach to diagnosis and management. By staying informed about the latest research and innovations in OHT, ophthalmologists can improve risk stratification, tailor treatment regimens to individual patient needs, and ultimately reduce the burden of glaucomatous vision loss.
For further reading and reference:
- American Academy of Ophthalmology – Ocular Hypertension: https://www.aao.org/eye-health/diseases/ocular-hypertension
- Glaucoma Research Foundation – Ocular Hypertension: https://www.glaucoma.org/glaucoma/ocular-hypertension.php
- National Eye Institute – Glaucoma: https://www.nei.nih.gov/learn-about-eye-health/eye-conditions-and-diseases/glaucoma


