Unraveling Peripheral Ulcerative Keratitis (PUK): Insights into Diagnosis and Management
Abstract: Peripheral Ulcerative Keratitis (PUK) stands as a sight-threatening ocular condition characterized by peripheral corneal thinning and ulceration, often associated with underlying systemic autoimmune diseases. This article delves into the intricacies of PUK, encompassing its clinical presentation, diagnostic criteria, associated systemic conditions, and therapeutic interventions, with a focus on preserving ocular integrity and preventing vision loss.
Introduction: Peripheral Ulcerative Keratitis (PUK) poses a diagnostic and therapeutic challenge due to its diverse etiologies and potential systemic implications. Understanding the underlying mechanisms and identifying associated systemic diseases are crucial steps in managing this vision-threatening condition effectively.
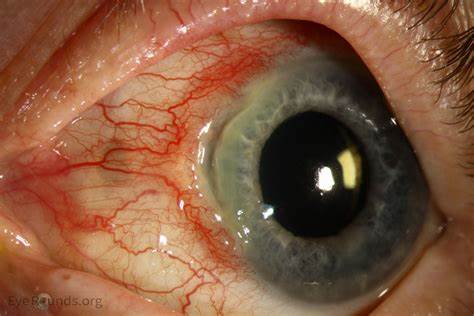
Clinical Presentation: PUK typically presents with peripheral corneal thinning, epithelial defects, and ulceration, accompanied by adjacent inflammatory infiltrates and stromal melting. Patients may experience symptoms such as ocular pain, redness, photophobia, and decreased vision, necessitating prompt ophthalmologic evaluation and management.
Diagnostic Criteria: Diagnosing PUK involves a comprehensive assessment of ocular findings, including slit-lamp examination, corneal imaging, and laboratory investigations. Ancillary tests such as corneal biopsy and systemic workup for autoimmune diseases aid in confirming the diagnosis and guiding treatment decisions.
Associated Systemic Conditions: PUK is often associated with systemic autoimmune diseases, including rheumatoid arthritis, systemic lupus erythematosus, Wegener’s granulomatosis, and polyarteritis nodosa. Timely recognition of these underlying conditions is essential for initiating appropriate systemic therapy and preventing systemic complications.
Therapeutic Interventions: The management of PUK aims to halt corneal melting, control inflammation, and address underlying systemic diseases. Treatment modalities may include topical and systemic corticosteroids, immunomodulatory agents, and systemic immunosuppressive therapy, tailored to the severity of ocular and systemic involvement.
Prognosis and Follow-Up: The prognosis of PUK depends on the underlying etiology, extent of corneal involvement, and response to treatment. Close monitoring of ocular inflammation, corneal integrity, and systemic disease activity is essential for optimizing visual outcomes and preventing disease recurrence.
Conclusion: Peripheral Ulcerative Keratitis (PUK) represents a complex interplay between ocular inflammation and systemic autoimmune diseases, necessitating a multidisciplinary approach to diagnosis and management. By recognizing early clinical signs, implementing timely interventions, and coordinating care with rheumatologists and other specialists, ophthalmologists can mitigate vision-threatening complications and improve patient outcomes in PUK.


