Unraveling the Complexities of Hypertensive Retinopathy: A Comprehensive Examination
Hypertensive retinopathy, a common ocular manifestation of systemic hypertension, encompasses a spectrum of retinal vascular changes that reflect the impact of elevated blood pressure on the microvasculature of the retina. This article endeavors to provide a thorough exploration of hypertensive retinopathy, delving into its pathophysiology, clinical manifestations, diagnostic approaches, management strategies, and prognostic implications.
Introduction: Hypertensive retinopathy serves as a critical indicator of systemic hypertension’s effects on the retinal microvasculature, offering valuable insights into a patient’s overall cardiovascular health and risk of end-organ damage. Understanding the nuances of hypertensive retinopathy is paramount for ophthalmologists and healthcare providers in effectively managing patients with systemic hypertension.
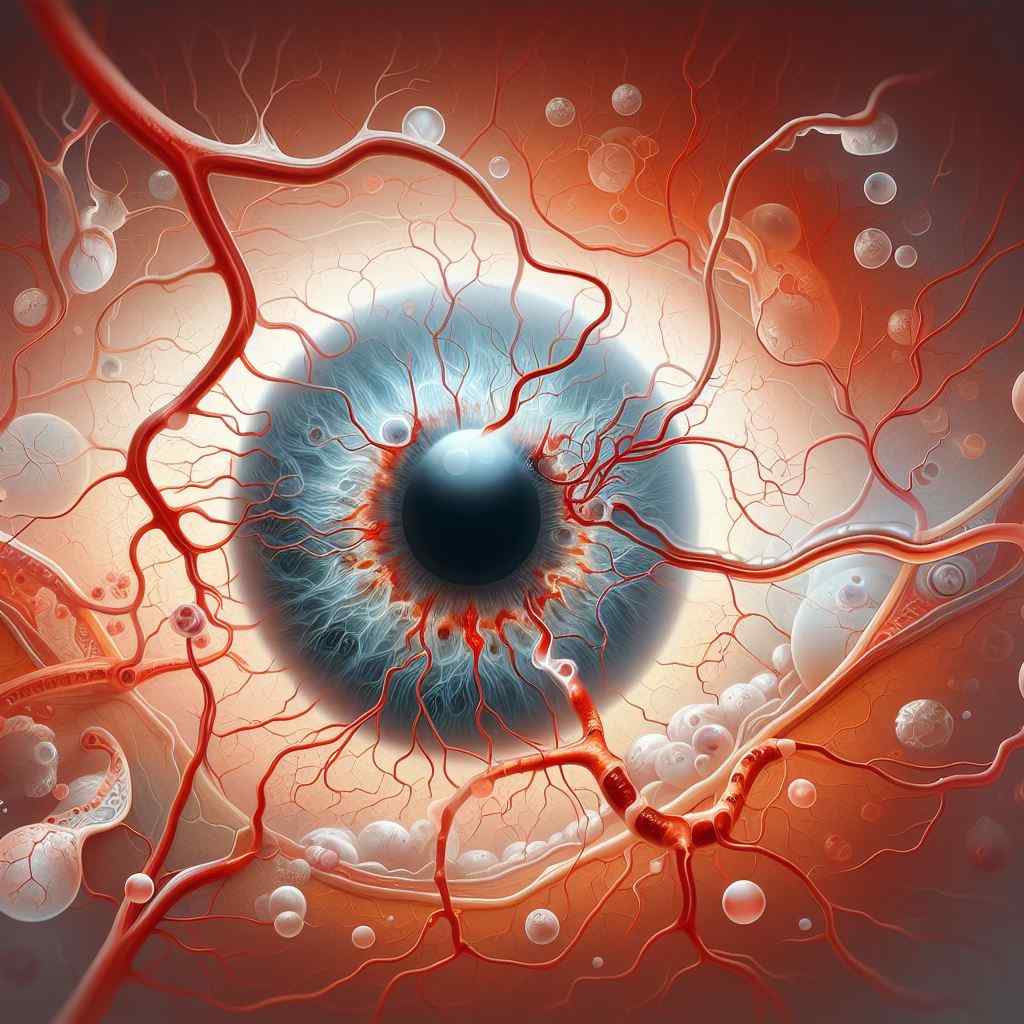
Pathophysiology: The pathophysiology of hypertensive retinopathy involves chronic hypertension-induced changes in retinal blood flow, vascular autoregulation, and endothelial dysfunction, leading to a cascade of microvascular alterations, including arteriolar narrowing, arteriovenous nicking, cotton-wool spots, retinal hemorrhages, and optic disc edema. These changes reflect the severity and duration of systemic hypertension and may progress with inadequate blood pressure control.
Clinical Manifestations: Clinical manifestations of hypertensive retinopathy encompass a spectrum of retinal findings that correlate with the severity and duration of systemic hypertension. These include arteriolar narrowing, copper or silver wiring, arteriovenous nicking, cotton-wool spots, retinal hemorrhages, macular edema, and optic disc changes such as swelling or pallor. Patients may be asymptomatic in the early stages, with symptoms manifesting as visual disturbances, headaches, or hypertensive emergencies in advanced cases.
Diagnostic Approaches: Diagnosing hypertensive retinopathy requires a comprehensive ophthalmic examination, including visual acuity assessment, funduscopy, and ancillary tests such as fundus photography, optical coherence tomography (OCT), fluorescein angiography (FA), and blood pressure monitoring. These diagnostic modalities aid in characterizing the extent and severity of retinal vascular changes, guiding treatment decisions and prognostic assessments.
Management Strategies: Management of hypertensive retinopathy centers on controlling systemic blood pressure through lifestyle modifications and pharmacological interventions to prevent further retinal vascular damage and mitigate the risk of cardiovascular complications. Treatment modalities may include antihypertensive medications, dietary modifications, weight management, smoking cessation, and regular exercise, tailored to individual patient needs and risk factors.
Prognostic Implications: The prognostic implications of hypertensive retinopathy extend beyond ocular health, serving as prognostic markers for systemic cardiovascular outcomes and mortality risk. Patients with advanced hypertensive retinopathy are at increased risk of cardiovascular events, stroke, and end-organ damage, underscoring the importance of early detection, aggressive blood pressure control, and multidisciplinary management in optimizing patient outcomes.
Conclusion: Hypertensive retinopathy represents a clinically significant manifestation of systemic hypertension, offering valuable insights into a patient’s overall cardiovascular health and prognosis. By elucidating the pathophysiology, clinical manifestations, diagnostic approaches, management strategies, and prognostic implications associated with hypertensive retinopathy, we can enhance our understanding of this complex ocular condition and improve patient care and outcomes.
Links:


